Pradhan Mantri Jan Arogya Yojana (PM-JAY)
Ayushman Bharat, a flagship scheme of Government of India, was launched as recommended by the National Health Policy 2017, to achieve the vision of Universal Health Coverage (UHC). This initiative has been designed to meet Sustainable Development Goals (SDGs) and its underlining commitment, which is to “leave no one behind.”
Ayushman Bharat is an attempt to move from sectoral and segmented approach of health service delivery to a comprehensive need-based health care service. This scheme aims to undertake path breaking interventions to holistically address the healthcare system (covering prevention, promotion and ambulatory care) at the primary, secondary and tertiary level. Ayushman Bharat adopts a continuum of care approach, comprising of two inter-related components, which are –
- Health and Wellness Centres (HWCs)
- Pradhan Mantri Jan Arogya Yojana (PM-JAY)
1. Health and Wellness Centers (HWCs)
In February 2018, the Government of India announced the creation of 1,50,000 Health and Wellness Centres (HWCs) by transforming the existing Sub Centres and Primary Health Centres. These centres are to deliver Comprehensive Primary Health Care (CPHC) bringing healthcare closer to the homes of people. They cover both, maternal and child health services and non-communicable diseases, including free essential drugs and diagnostic services.
Health and Wellness Centers are envisaged to deliver an expanded range of services to address the primary health care needs of the entire population in their area, expanding access, universality and equity close to the community. The emphasis of health promotion and prevention is designed to bring focus on keeping people healthy by engaging and empowering individuals and communities to choose healthy behaviours and make changes that reduce the risk of developing chronic diseases and morbidities.
2. Pradhan Mantri Jan Arogya Yojana (PM-JAY)
The second component under Ayushman Bharat is the Pradhan Mantri Jan Arogya Yojana or PM-JAY as it is popularly known. This scheme was launched on 23rd September, 2018 in Ranchi, Jharkhand by the Hon’ble Prime Minister of India, Shri Narendra Modi.
Ayushman Bharat PM-JAY is the largest health assurance scheme in the world which aims at providing a health cover of Rs. 5 lakhs per family per year for secondary and tertiary care hospitalization to over 12 crores poor and vulnerable families (approximately 55 crore beneficiaries) that form the bottom 40% of the Indian population. The households included are based on the deprivation and occupational criteria of Socio-Economic Caste Census 2011 (SECC 2011) for rural and urban areas respectively. PM-JAY was earlier known as the National Health Protection Scheme (NHPS) before being rechristened. It subsumed the then existing Rashtriya Swasthya Bima Yojana (RSBY) which had been launched in 2008. The coverage mentioned under PM-JAY, therefore, also includes families that were covered in RSBY but are not present in the SECC 2011 database. PM-JAY is fully funded by the Government and cost of implementation is shared between the Central and State Governments.
Key Features of PM-JAY
- PM-JAY is the world’s largest health insurance/ assurance scheme fully financed by the government.
- It provides a cover of Rs. 5 lakhs per family per year for secondary and tertiary care hospitalization across public and private empanelled hospitals in India.
- Over 12 crore poor and vulnerable entitled families (approximately 55 crore beneficiaries) are eligible for these benefits.
- PM-JAY provides cashless access to health care services for the beneficiary at the point of service, that is, the hospital.
- PM-JAY envisions to help mitigate catastrophic expenditure on medical treatment which pushes nearly 6 crore Indians into poverty each year.
- It covers up to 3 days of pre-hospitalization and 15 days post-hospitalization expenses such as diagnostics and medicines.
- There is no restriction on the family size, age or gender.
- All pre–existing conditions are covered from day one.
- Benefits of the scheme are portable across the country i.e. a beneficiary can visit any empanelled public or private hospital in India to avail cashless treatment.
- Services include approximately 1,929 procedures covering all the costs related to treatment, including but not limited to drugs, supplies, diagnostic services, physician’s fees, room charges, surgeon charges, OT and ICU charges etc.
- Public hospitals are reimbursed for the healthcare services at par with the private hospitals.
Benefit Cover Under PM-JAY
Benefit cover under various Government-funded health insurance schemes in India have always been structured on an upper ceiling limit ranging from an annual cover of INR30,000 to INR3,00,000 per family across various States which created a fragmented system. PM-JAY provides cashless cover of up to INR5,00,000 to each eligible family per annum for listed secondary and tertiary care conditions. The cover under the scheme includes all expenses incurred on the following components of the treatment.
- Medical examination, treatment and consultation
- Pre-hospitalization
- Medicine and medical consumables
- Non-intensive and intensive care services
- Diagnostic and laboratory investigations
- Medical implantation services (where necessary)
- Accommodation benefits
- Food services
- Complications arising during treatment
- Post-hospitalization follow-up care up to 15 days
The benefits of INR 5,00,000 are on a family floater basis which means that it can be used by one or all members of the family. The RSBY had a family cap of five members. However, based on learnings from those schemes, PM-JAY has been designed in such a way that there is no cap on family size or age of members. In addition, pre-existing diseases are covered from the very first day. This means that any eligible person suffering from any medical condition before being covered by PM-JAY will now be able to get treatment for all those medical conditions as well under this scheme right from the day they are enrolled.

Why PM-JAY: A Background
Over the last few decades, the world’s eyes have been on India as it’s economy has been one of the top three fastest growing economies of the world. However, despite making remarkable strides in several sectors, India is still classified as a Lower Middle-Income Country (LMIC) according to World Bank classification of countries based on per capita GDP, mostly due to its inconsistent socio-economic and health indicators.
Statistics show that more than 20 per cent of India’s population still lives under $1.9 per day (2011 PPP). According to a World Bank projection, by 2021 more than 34% of India’s population will be in the age group of 15-35 years. This rich demographic dividend enables India to be highly optimistic about a sustained economic growth for few more decades before a higher dependency ratio sets in. However, the perceived benefits of the higher demographic dividend are threatened by the epidemiological transition in India which is currently facing the unique situation of a “triple burden of disease.” As the mission of eradication of major communicable diseases remains unfinished, the population is also bearing the high burden of non-communicable diseases (NCDs) and injuries. This leads to an overall rise in the demand for health care over a prolonged period of time.
However, with a total population of more than 1.3 billion people, the supply side of adequate and affordable healthcare in India is found wanting. Figures show an overwhelming tilt towards health care services in the private sector which cater to nearly 70% of all visits for health care needs in India and have 50% of total hospital beds. But, individually most providers in the private sector are very small (with less than 25 beds). They are also unregulated, with varying standards of quality of care and are mostly situated in large metros or urban neighbourhoods leaving a great deficit of health services for the underprivileged population of India.
But being the second most populous nation in the world, the public sector hospitals in India are understandably overburdened. Their utilisation varies widely and they often have to work under challenging circumstancing arising from the lack of sufficient funds, a shortage of trained health workers and the erratic and often deficient supply of drugs and equipment which adversely impacts their functioning.
One of the major causes of this situation is the persistent underfunding of the country’s public health care system. Over the last two decades, the Government of India’s overall expenditure on health has remained stagnant at about 1.2% of its GDP (Source: National Health Accounts, 2015). Of its total expenditure on health, India spends only 21% from the Government revenue and as high as 62% from out-of-pocket expenses (Source: National Health Accounts, 2015). Thus, it has been deduced that increasing health care needs, coupled with high out-of-pocket expenditure, is a leading cause of poverty in India. Not only does it keep people poor, but it also pushes nearly 6 crore Indians back into poverty each year. The following graph depicts this situation clearly by comparing the OOP to total expenditure on health in two decades.

In the past, there have been several efforts by the Central and various State Governments to strengthen demand side financing by launching various Government-funded health insurance schemes. The Rashtriya Swasthya Bima Yojana (RSBY) was launched with an annual cover of INR30,000 per family at the central level which catered mostly to secondary care hospitalisation while many State schemes catered to tertiary care conditions. However, these schemes worked independently of the larger health care system in the country and resulted in further increasing the fragmentation of risk pools. Additionally, none of these schemes had any linkage with primary health care.
To address these challenges, the Government of India took a two-pronged approach under the umbrella of Ayushman Bharat. The first component of this strategy was disease prevention and health promotion to curb the increasing epidemic of non-communicable diseases. This was to be ensured through upgradation of the existing network of Sub-centres and Primary Health Centres to Health and Wellness Centres (HWC). Nearly 150,000 HWCs are to be set up in the country over the next few years which will work towards reducing the overall disease burden and hospitalisation needs of the population.
The second component was the launch of the Pradhan Mantri-Jan Arogya Yojana (PM-JAY) which aims to create a system of demand-led health care reforms that meet the immediate hospitalisation needs of the eligible beneficiary family in a cashless manner thus insulating the family from catastrophic financial shock. In the long run, the PM-JAY, through its system of incentives, aims to expand the availability of its services. With greater demand, the private sector is likely to expand in the unserved areas of Tier-2 and Tier-3 cities. For public hospitals, PM-JAY will provide an incentive to prioritise poor patients and shall provide means to generate additional revenue for strengthening their infrastructure and fill their service gaps. PM-JAY has subsumed the existing RSBY and also works in convergence with various State Government funded health insurance/ assurance schemes.
Because of its scope, PM-JAY is the world’s largest health insurance/assurance scheme that offers a health cover to nearly 12 crore poor families which comes to a staggering 55 crore Indians that form 40% of its bottom population. It is fully funded by the Government and provides financial protection for a wide variety of secondary and tertiary care hospitalisations. The prime objective of PM-JAY is to reduce catastrophic out-of-pocket health expenditure by improving access to quality health care for its underprivileged population. More details on its evolution, planning, eligibility and state wise implementation are discussed ahead.
Coverage under PM-JAY
Including the poorest and most vulnerable population of any country in the health insurance programme is often the most challenging because they cannot pay any premium and are the hardest to reach. Many times they are also not literate and, therefore, require a very different approach for awareness generation. This is true for most Lower and Middle-Income Countries (LMIC) and India is not an exception.
Thus, PM-JAY has been rolled out for the bottom 40 per cent of poor and vulnerable population. In absolute numbers, this is close to 12 crore households. The inclusion of households is based on the deprivation and occupational criteria of the Socio-Economic Caste Census 2011 (SECC 2011) for rural and urban areas, respectively. This number also includes families that were covered in the RSBY but were not present in the SECC 2011 database.
The SECC involves ranking of the households based on their socio-economic status. It uses exclusion and inclusion criteria and accordingly decides on the automatically included and automatically excluded households. Rural households which are included (not excluded) are then ranked based on their status of seven deprivation criteria (D1 to D7). Urban households are categorised based on occupation categories.
In line with the approach of the Government to use the SECC database for social welfare schemes, PM-JAY also identifies targeted beneficiary families through this data.
Out of the total seven deprivation criteria for rural areas, PM-JAY covered all such families who fall into at least one of the following six deprivation criteria (D1 to D5 and D7) and automatic inclusion(Destitute/ living on alms, manual scavenger households, primitive tribal group, legally released bonded labour) criteria:
- D1- Only one room with kucha walls and kucha roof
- D2- No adult member between ages 16 to 59
- D3- Households with no adult male member between ages 16 to 59
- D4- Disabled member and no able-bodied adult member
- D5- SC/ST households
- D7- Landless households deriving a major part of their income from manual casual labour
Urban Beneficiaries
For urban areas, the following 11 occupational categories of workers are eligible for the scheme:
- Ragpicker
- Beggar
- Domestic worker
- Street vendor/ Cobbler/hawker / other service provider working on streets
- Construction worker/ Plumber/ Mason/ Labour/ Painter/ Welder/ Security guard/ Coolie and other head-load worker
- Sweeper/ Sanitation worker/ Mali
- Home-based worker/ Artisan/ Handicrafts worker/ Tailor
- Transport worker/ Driver/ Conductor/ Helper to drivers and conductors/ Cart puller/ Rickshaw puller
- Shop worker/ Assistant/ Peon in small establishment/ Helper/Delivery assistant / Attendant/ Waiter
- Electrician/ Mechanic/ Assembler/ Repair worker
- Washer-man/ Chowkidar
Even though PM-JAY uses the SECC as the basis of eligibility of households, many States are already implementing their own health insurance schemes with a set of beneficiaries already identified. Thus, States have been provided the flexibility to use their own database for PM-JAY. However, they will need to ensure that all the families eligible based on the SECC database are also covered.
Expansion of coverage by States under PM-JAY and convergenceVarious States have been implementing their own health insurance/assurance schemes over the past couple of decades. Most of these schemes provide cover for tertiary care conditions only. The benefit cover of these schemes is mostly available within the State boundaries except some smaller States have empanelled a few hospitals outside the State boundaries. Very few States had converged their schemes with the erstwhile RSBY scheme and many of them were operating independently. This was due to the lack of flexibility in the design of the RSBY, which although initially helped in quick scale-up but became a challenge over a period of time and offered limited flexibility to the States.
Even though these schemes were targeting the poor and vulnerable, there were large variations across States in terms of eligibility criteria and databases. Few States were using the food subsidy database while some others had created a separate database for their welfare schemes.
The primary objectives for launching PM-JAY were to ensure comprehensive coverage for catastrophic illnesses, reduce catastrophic out-of-pocket expenditure, improve access to hospitalisation care, reduce unmet needs, and to converge various health insurance schemes across the States. PM-JAY will also establish national standards for a health assurance system and is providing national portability of care. At the implementation level, the States are given the flexibility to use their own database if they were already implementing a health insurance/ assurance scheme and were covering more families than those eligible as per the SECC 2011 database. However, such States shall ensure that all families eligible as per the SECC data are covered and not denied benefits.
Various States are using different models for implementing their own health insurance/ assurance schemes. Some of them are using the services of insurance companies while others are directly implementing the schemes in their States. Considering the fact that States are at different levels of preparedness and have varying capacity to manage such schemes, PM-JAY provides the States with the flexibility to choose their implementation model. They can implement scheme through assurance/trust model, insurance model or mixed model.
A. Assurance Model/Trust Model This is the most common implementation model adopted by most of the States. Under this model, the scheme is directly implemented by the SHA without the intermediation of the insurance company. The financial risk of implementing the scheme is borne by the Government in this model. SHA essentially reimburses health care providers directly. Even though no insurance company is involved, the SHA employ the services of an Implementation Support Agency (ISA) for claim management and related activities. As there is no insurance company in the picture, apart from day-to-day management and administration of the scheme, the SHA also has to carry out specialised tasks such as hospital empanelment, beneficiary identification, claims management and audits and other related tasks
B. Insurance Model In the insurance model, the SHA competitively selects an insurance company through a tendering process to manage PM-JAY in the State. Based on market determined premium, SHA pays premium to the insurance company per eligible family for the policy period and insurance company, in turn, does the claims settlement and payments to the service provider. The financial risk for implementing the scheme is also borne by the insurance company in this model. However, to ensure that the insurance company does not make an unreasonable profit, the scheme provides for a mechanism where insurance companies can only get a limited percentage of the premium for their profit and administrative costs. After adjusting a defined percentage for expenses of management (including all costs excluding only service tax and any cess, if applicable) and after settling all claims, if there is surplus then 100 per cent of leftover surplus should be refunded by the insurer to the SHA within 30 days. The percentage that will need to be refunded will be as per the following: a. In Category A States (administrative cost cannot exceed 20%)
- i. Administrative cost allowed 10% if claim ratio less than 60%.
- ii. Administrative cost allowed 15% if claim ratio between 60 to less than 70%.
- iii. Administrative cost allowed 20% if claim ratio between 70 to less than 80%.
- i. Administrative cost allowed 10% if claim ratio less than 60%.
- ii. Administrative cost allowed 12% if claim ratio between 60 to less than 70%.
- iii. Administrative cost allowed 15% if claim ratio between 70 to less than 85%.
C. Mixed Model Under this, the SHA engages both the assurance/ trust and insurance models mentioned above in various capacities with the aim of being more economic, efficient, providing flexibility and allowing convergence with the State scheme. This model is usually employed by brownfield States which had existing schemes covering a larger group of beneficiaries.
| Category A States/ UTs | Arunachal Pradesh, Goa, Himachal Pradesh, Jammu and Kashmir, Manipur, Meghalaya, Mizoram, Nagaland, NCT Delhi, Sikkim, Tripura, Uttarakhand and 6 Union Territories (Andaman and Nicobar Islands, Chandigarh, Dadra and Nagar Haveli, Daman and Diu, Lakshadweep and Puducherry) |
| Category B States | Andhra Pradesh, Assam, Bihar, Chhattisgarh, Gujarat, Haryana, Jharkhand, Karnataka, Kerala, Madhya Pradesh, Maharashtra, Odisha, Punjab, Rajasthan, Tamil Nadu, Telangana, Uttar Pradesh and West Bengal |
Financing of the Scheme
PM-JAY is completely funded by the Government and costs are shared between Central and State Governments. The Government of India decides a national ceiling amount per family that is used to determine the maximum limit of the central share of the contribution. The actual premium discovered through open tendering process or the maximum ceiling of the estimated premium decided by Government of India for the implementation of PM-JAY, whichever is less, would be shared between Central Government and States/UTs in the ratio as per the extant directives issued by Ministry of Finance, from time to time. In addition, administrative cost for implementing the scheme at the State level is also provided under the scheme and shared between Centre and State in the same sharing pattern.
The existing sharing pattern is in the ratio of 60:40, for States (other than North-Eastern States & three Himalayan States) and Union Territories with legislature. For North-Eastern States and three Himalayan States (viz. Jammu and Kashmir, Himachal Pradesh and Uttarakhand), the ratio is 90:10. For Union Territories without legislatures, the Central Government may provide up to 100% on a case-to-case basis.
Payment of Central Share- Insurance model – A flat premium per family, irrespective of the number of members under PM-JAY in that family, is paid to the State Government which in turn pays this to the insurer based on the number of eligible families.
- Assurance model – Central share of the contribution is paid based on the actual cost of claims or the ceiling whichever is lower. If the State is using an Implementation Support Agency, then cost of ISA, determined through tender, is also shared between Centre and State.
Expansion of Coverage By States Under PM-JAY, Convergence and Flexibility to The States
Various States have been implementing their own health insurance/assurance schemes over the past couple of decades. Most of these schemes provide cover for tertiary care conditions only. The benefit cover of these schemes is mostly available within the State boundaries except some smaller States who have empanelled a few hospitals outside the State boundaries. Very few States had converged their schemes with the erstwhile RSBY scheme and many of them were operating independently. This was due to the lack of flexibility in the design of the RSBY, which although initially helped in quick scale-up but became a challenge over a period of time and offered limited flexibility to the States.
Even though these schemes were targeting the poor and vulnerable, there were large variations across States in terms of eligibility criteria and databases. Few States were using the food subsidy database while some others had created a separate database for their welfare schemes.
The primary objectives for launching PM-JAY were to ensure comprehensive coverage for catastrophic illnesses, reduce catastrophic out-of-pocket expenditure, improve access to hospitalisation care, reduce unmet needs, and to converge various health insurance schemes across the States. PM-JAY will also establish national standards for a health assurance system and is providing national portability of care.
In the spirit of cooperative federalism and keeping in mind variations across the States, a lot of flexibility has been built in the PM-JAY design. Therefore, PM-JAY provides a lot of flexibility to States in terms of scheme design and implementation.
States have been provided the flexibility in terms of the following parameters:- Mode of implementation – States can choose the implementation model and can implement the scheme through Trust, Insurance company or Mixed model.
- Usage of beneficiary data – PM-JAY uses SECC data for targeting the beneficiaries, however, States have been provided flexibility to decide on the dataset for this purpose, if they are covering more beneficiaries than SECC defined numbers. However, State will need to ensure that all beneficiaries eligible as per SECC data are also covered.
- Co-branding – States can co-brand their existing health insurance/assurance schemes with PM-JAY as per co-branding guidelines of the scheme.
- Expansion of cover to more people – States can cover more number of families than those defined as per SECC data. For these additional families, full cost will need to be borne by the States.
- Increasing benefit cover to higher value – If the State want they can even expand the benefit cover beyond `5 lakh per family per year. However, in this case cost of additional cover will need to be completely borne by the State.
- Revision in package numbers and pricing – PM-JAY provides cover of more than 1300 packages and their prices have been fixed by NHA. However, keeping in view the different disease profile and cost of services variations across the States, flexibility has been provided to the States to expand the number of packages and also within a limit State can also revise the package prices.
- Reservation of packages for public hospitals – To ensure that such services that can be provided well by Government health facilities are not misused by private providers, NHA has defined a set of conditions that are reserved for only public health care facilities. States can revise list of such conditions that are reserved for public hospitals.
- IT Systems – Before the launch of PM-JAY some of the States were implementing their own health insurance schemes and were using their own IT systems. PM-JAY provides flexibility that State can continue using their own IT system and share data with NHA on a real time basis in specified format.
- Payment to public hospitals – States have also been provided flexibility to deduct a certain percentage of claims amount that is paid to public hospitals.
Hospital Empanelment
The supply of health care services under PM-JAY must be ensured through pre-selected, well equipped and well-prepared hospitals to deliver the benefits. Also, the hospitals must be distributed widely enough over the geography so as to ensure optimal accessibility to the eligible families.
In order to cater to the increased demands under PM-JAY and also to ensure quality care to the beneficiaries, it is imperative to maintain and grow a network of hospitals that also conform to the quality standards and criteria. This leads to the need of empanelment of hospitals on a pre-emptive basis so that beneficiaries are certain of their rights being honoured in the most convenient, cashless and quality manner.
Empanelment CriteriaConsidering the supply side characteristics (nearly 71 per cent of the hospitals are running as proprietorship businesses with less than 25 beds capacity and offering non-specialised general clinical care), two types of empanelment criteria have been evolved. These criteria have been evolved based on the experience of the prevalent practice in other Government-funded health insurance schemes, State-specific regulations related to the quality of care and Clinical Establishment Act 2011.
The detailed criteria for empanelment are available on www.pmjay.gov.in
- General criteria – For hospitals that provide non-specialised general medical and surgical care with or without ICU and emergency services.
- Special Criteria (for clinical specialties) – For each specialty, a specific set of criteria has been identified. Under PM-JAY, a hospital is not allowed to select the risk, which means it cannot apply for selected specialties and must agree to offer all specialties to PM-JAY beneficiaries that are offered by it. However, in order to offer a specialised clinical service, the hospital must have necessary specific infrastructure and HR in place as mentioned in the special criteria developed under PM-JAY for the same.
Process of hospital empanelment in PM-JAY
PM-JAY prescribes a two-tier approach to the empanelment of hospitals which is online, transparent and efficient and is completely free for all steps of the process. States are in the stewardship position of the entire process of hospital empanelment and they have the final decision-making power in this regard. At the State level, a State Empanelment Committee (SEC) has been set up under the State Health Agency. At the district level, a District Empanelment Committee (DEC) has been set up.
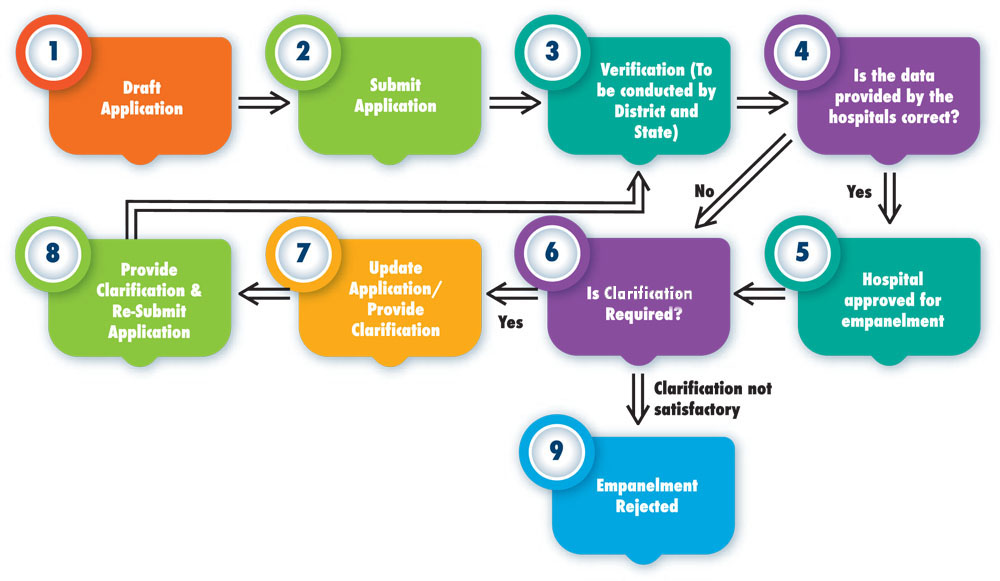
Each empanelled hospital needs to set up a dedicated help desk for the beneficiaries, which is manned by a dedicated staff appointed by the Empanelled Health Care Provider (EHCP). These help desk staff are called Pradhan Mantri Arogya Mitras (PMAMs) and their role is to facilitate treatment of beneficiaries at the hospitals. Every empanelled hospital receives a unique ID also.
- Hospitals are required to apply online which is free of cost. The progress of the application can also be tracked online.
- The online applications are scrutinised by the DEC and physical verification of the hospitals is carried out.
- Following this verification, the DEC submits a recommendation to approve or reject the hospital to the SEC. The final decision regarding empanelment rests with the SEC.
Continuous quality improvement and other incentives to empanelled hospitals
PM-JAY incentivises the empanelled hospitals to continuously strive for the attainment of higher quality standards. These incentives are certainly a motivation for the hospitals to attain the said quality standards. The following incentives are being provided under PM-JAY to the hospitals over and above the package rates
- At the time of empanelment a hospital need not be NABH accredited but if during the course of association with PM-JAY a hospital attains entry level NABH accreditation, it is paid 10 per cent higher package rates. Similarly, the hospital attaining a full accreditation is paid 15 percent higher.
- Hospitals attached to teaching institutions (medical, PG and DNB courses) are entitled for 10 per cent higher packages.
- Also, to promote the hospitals to reach out to the beneficiaries in underserved areas, PM-JAY has come up with 10% higher package rates for hospitals which are situated in aspirational districts.
National Health Care Providers (NHCP)
Although States are in charge of the empanelment of hospitals, there are eminent tertiary care hospitals and specialised care hospitals that operate as autonomous institutes of excellence directly under the Ministry of Health and Family Welfare (MoHFW) or some other department. Most popular examples of such hospitals are AIIMS, Safdarjang Hospital, JIPMER, PGI Chandigarh, etc. The National Health Authority (NHA) has empanelled these hospitals directly by signing an MoU with each of the facility. Also, all NABH accredited private hospitals in the National Capital Region (NCR) are directly empanelled by NHA to widen the network of service providers. Empanelment of Government hospitals other than those managed by MoHFW is also a major step towards widening the network of hospitals.
Packages and Rates
To ensure that the hospitals do not overcharge and rates do not vary across hospitals, empanelled health care providers (EHCP) are paid based on specified package rates. A package consists of all the costs associated with the treatment, including pre and post hospitalisation expenses. The specified surgical packages are paid as bundled care (explained below) where a single all-inclusive payment is payable to the EHCP by insurer/SHA. The medical packages, however, are payable to the EHCP on a per day rate depending upon the admission unit (general ward, HDU, ICU) with certain pre-decided add-ons payable separately. Day-care packages are payable just like surgical packages. The treatment packages are very comprehensive, covering treatment for nearly 24 specialities that include super speciality care like oncology, neurosurgery and cardio-thoracic and cardiovascular surgery, etc. The package rate (in case of surgical or defined day-care benefits) includes:
- Registration charges
- Bed charges (General Ward)
- Nursing and Boarding charges
- Surgeons, Anaesthetists, Medical Practitioner, Consultants’ fees, etc.
- Anaesthesia, Blood Transfusion, Oxygen, O.T. Charges, Cost of Surgical Appliances, etc.
- Medicines and Drugs
- Cost of Prosthetic Devices, implants (unless payable separately)
- Pathology and radiology tests: radiology to include but not be limited to X-ray, MRI, CT Scan, etc. (as applicable)
- Food to patient
- Pre and Post Hospitalisation expenses: Expenses incurred for consultation, diagnostic tests and medicines before the admission of the patient in the same hospital, and up to 15 days of the discharge from the hospital for the same ailment/ surgery
- Any other expenses related to the treatment of the patient in the EHCP
As mentioned in the previous section based on a few criteria, hospitals can be paid a higher amount. For such surgical conditions that are not listed in the package list, an EHCP will need to take approval and fix the rate from the insurer/ SHA before providing the treatment up to the limit of INR 1,00,000.
Journey from HBP 1.0 to HBP 2.0
Soon after rollout, NHA started receiving feedback from stakeholders and various other sources on different aspects of AB PM-JAY including HBP 1.0. Majority of the feedback received on HBP could be broadly clubbed under the following heads:
- Package rates offered for many packages were inadequate to cover the cost of procedures
- Duplication of packages was observed both within a single specialty and across specialties
- The terminology used for the nomenclature of packages was inconsistent
- Few of the procedures were overlapping with the ongoing National Health Programs
- Some of the high-end procedures / investigations / drugs are not covered in HBP 1.0
- Due to the non-availability of certain treatments, a lot of procedures were being booked under Unspecified packages
Development of packages and rates under HBP 2.0
All the concerns and feedback received from stakeholders and various other sources of different aspects of AB PM-JAY were deliberated upon in the first Governing Board meeting of NHA, in the month of April 2019. To address the gross anomalies, a mandate was given to NHA for rationalization of HBP.
For this purpose, 24 Specialist Committees were constituted. A Memorandum of Understanding was inked between NHA and Tata Memorial Hospital (TMH) for the review of Oncology packages. Department of Health Research (DHR) was conducting a study “Costing of Health Services in India” (CHSI), the data collection from Public sector hospitals for 8 specialties had been completed. DHR agreed to share these interim results with NHA. These results were provided to the specialist committees as an input during deliberations for the rationalization of HBP pricing (Please see Annex 1: Inputs provided to the specialist committee and decisions sought). The initial steps in the exercise of rationalization of Health Benefit Package (HBP) were carried out using three different processes which are detailed in flow chart – “Process for rationalization of HBP”.
Following the due procedure, the recommendations were presented to the Governing Board of NHA. The Governing Board of NHA approved following changes:
- Increase in price of 270 packages
- Decrease in price of 57 packages
- Retain the price of 469 packages at original level
- Introduction of 237 new packages
- Stratification of 43 existing packages
- Discontinuation of 554 existing packages
- To discontinue the packages of Tubectomy and Vasectomy as the services are provided under National Family Welfare Program.
- The packages for Cataract were decided to be continued taking into account the existing disease burden and country’s commitment to reduce the prevalence of Cataract blindness
- It was decided by the Governing Board that the increase in package rates of 270 packages will be moderated by 10%.
Flexibility to States on packages
States with a State-owned health insurance scheme can keep their own rates for all the packages. However, they are required to adhere to mandatory 1,391 packages as specified in the PM-JAY list. The list can be expanded based on additional packages from their own scheme which were not a part of the national package master.
States with no health scheme other than PM-JAY can adopt the national package master with context-specific variations such as revision of prices in the range of 10 per cent, reservation of procedures for public hospitalisation, additional packages under mandatory pre-authorisation, etc. States do have the flexibility to add packages or modify rates according to their requirements; further, they even have the flexibility to change terms of pre-authorization and modify the list of the public hospital only packages which was devised to prevent any misuse. to see the revised list of Health Benefit Packages
Click here to see the revised list of Health Benefit PackagesAdvantages of HBP 2.0
- HBP 2.0 has features that facilitates an enhanced coverage of both disease conditions and procedures than were previously included, while keeping a low count of packages. Features which aid this enhanced coverage are stratification, cross specialty packages, multiple procedures in a package etc. This is expected to reduce the burden on PMAMs in selection of packages without compromising on data availability for analysis
- Certain packages are now allowed to be booked with a primary package at a 100% reimbursement contrary to the principle of 50% reimbursement of the second package in HBP 1.0. Also, some packages have been identified as Stand-Alone Packages which means that they cannot be booked with any other package.
- Some procedures require prolonged / multiple follow up beyond the limit of 15 days included in a package. For such procedures, follow – up packages have been included to ensure continuity of care.
- Certain features have been introduced in HBP 2.0 to minimise potential of fraud and abuse. In certain cases, time interval for booking of sequential packages has been defined, maximum number of permissible implants has been built in, maximum number of times a package can be booked in an individual has been defined. Other features such as identification of stand-alone packages, and standardization of rates across specialties is expected to further reduce incentives for upcoding.
- The HBP 2.0 features a 3-layered IT customization for easier and more accurate package booking. This allows better analytics and improved dashboards of package utilization and its monitoring. Scientific nomenclature and coding further strengthen HBP 2.0 towards uniformity and improved acceptance across the country.
IT System under PM-JAY
In order to enable PMJAY ‘swiftly & effortlessly,’ it was required that information technology is orchestrated in such as a manner that there is minimum ‘time-to-launch’. Since its launch IT has provided a robust backbone to the scheme’s implementation throughout the nation. The below are the key technology blocks.
Key Technology Blocks


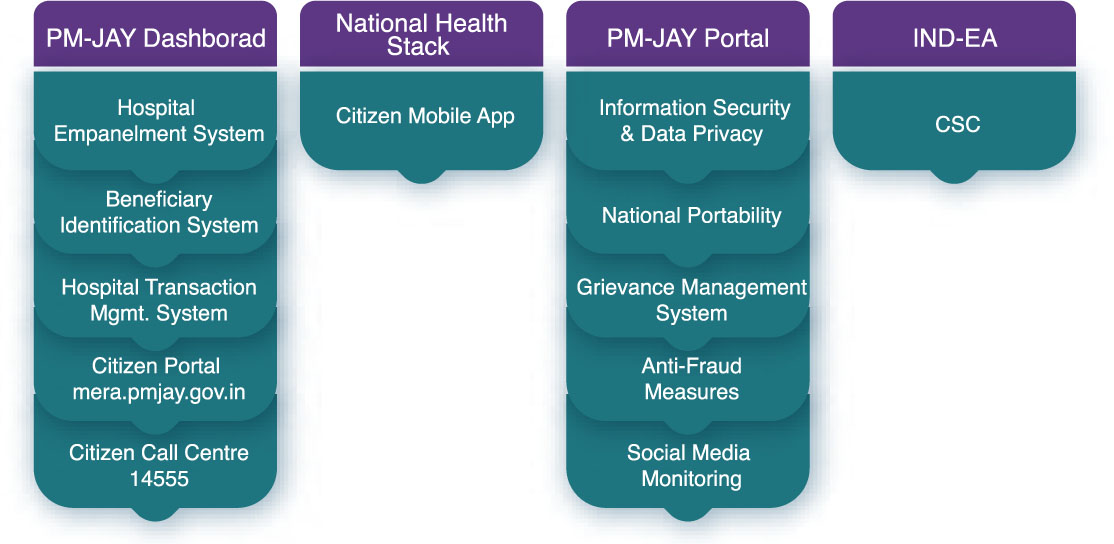
- PMJAY Dashboard :Allows for an aggregated and drill-down view on various datasets integrated into the PMJAY Data Warehouse. Is used for real-time reporting of transactions, evaluating performance and understanding utilization trends.
- Hospital Empanelment System :Allows for registration and approval of hospitals for empanelment. Features for Hospital Quality Assurance are also being made available in this system.
- Beneficiary Identification System (BIS) :Allows for searching beneficiaries through SECC or additional data sets through APIs and supports Aadhaar eKYC (electronic Know Your Customer) and non-Aadhaar based KYC for Authentication.
- Transaction Management System (TMS) :Allows for capturing of in-patient data on admission, treatment and discharge, and onwards to hospital claims and financial settlement. It is integrated with other State based and external systems through Application Program Interface (APIs).
- Citizen Portal (mera.pmjay.gov.in) :Allows for citizens to search the beneficiary database to ascertain the eligibility under the scheme. The popular self-help tool has allowed for mass scale searches right at the field level being mobile responsive.
- Citizen Call Centre (14555) :National Toll-Free number backed with a 400+ multi-lingual, multi-location call centre services which allows beneficiaries to find out their eligibility, nearest hospital, nearest Common Service Centre etc. Service offerings through the call centre have been enlarged to allow for beneficiary feedback and grievance redressal.
- National Health Stack :Followed as a design philosophy, the NHS shall enable PM-JAY to capture data which can be used in the future to enhance scheme design and allow for further inclusion/ universalization. Developments underway for National Health Claims Platform (NHCP) and enhancement of existing PM-JAY systems. These constructs will pave the way for creation of market led service delivery products for regulated insurance scheme.
- PM-JAY Portal :Single source of all information and content related to the scheme, the platform is being enhanced to support back-office functions as well. The portal is used to share best-practices, Standard Operating Procedures (SOPs), Policies and Guidelines, and act as a front end to the Grievance Management System.
- India Enterprise Architecture (IND-EA):Followed as a principle to enable development of a future ready enterprise architecture for PM-JAY and NHA.
- Information Security & Data Privacy Policies :Put in perspective the various check-lists enforced on the IT Ecosystem – Service Providers and Consumers to ensure end to end information security and privacy of personally identifiable data for beneficiaries. Continuous assessments are undertaken to ensure compliance.
- National Portability :Unique to the scheme, IT system has allowed portability of benefits for the beneficiary regardless of the location. This has been possible only by designing systems which allow for a real-time integration and data-exchange across the IT landscape.
- Grievance Management System :Allows for beneficiaries and whistle-blowers to register grievances and for NHA/ SHAs to ‘take-to-closure’ such grievances. As a key element towards building trust amongst beneficiaries, the system ensures anonymity of the griever.
- Anti-Fraud Measures :As part of the IT landscape, a ‘Man-Machine’ model has been envisaged to counter fraudulent transactions and entities. The model shall generate triggers for suspicious transactions and entities, and will also allow for closure of investigations of such transactions. National Anti-Fraud Unit and State Anti-Fraud Unit have been institutionalized to support investigations at the State level.
- Citizen Mobile App :Allows for registered beneficiaries to find out their existing ‘wallet balance’ in the scheme, search for the nearest hospitals and provide feedback on the services being provided by the hospitals. As a simple personal tool shall empower the beneficiaries to know their utilization of the entitled benefits.
- Common Service Centre (CSC) :As a service delivery partner, CSCs further the reach of the scheme in rural India through their Gram Panchayat level network. CSCs have helped extensively through their network in not only communicating about the scheme but also helping potential beneficiaries find out about their eligibility and authenticating eligible beneficiaries.
- B. PM-JAY IT Ecosystem


Awareness and Communication
Since PM-JAY is an entitlement-based scheme where there is no advance enrolment process, making beneficiaries aware of the scheme is the most critical aspect. Information, Education and Communication activities need to be carried out to educate beneficiaries about the scheme. Various modes of communication such as leaflets, booklets, hoardings, TV, radio spots etc are important elements for creating a comprehensive communication strategy for disseminating the desired messages across the target audience.
A detailed communication strategy has been developed by NHA which is to be implemented at both national and State levels. NHA is also working on the overall cooperation & capacity-building with the States for implementation and development of communication strategy required for increasing awareness at the State level.
Due to large quantum of people being covered under PM-JAY, there is a strong need to spread awareness with the right message, through the right media and within the right timeframe. IEC activities were initiated immediately after the Cabinet approval to the scheme on 21st March, 2019. The first major initiative, Additional Data Collection Drive (ADCD) drive was undertaken by participating in “Gram Swaraj Abhiyaan” of Ministry of Rural Development on 30th April, 2018 named as “Ayushman Bharat Diwas” with an objective to make people aware about the upcoming scheme benefits and entitlement check by involving ASHA & ANMs and Gram Sevak covering around 3 lakh villages across the country. Various posters, banners etc. were designed and deployed in Hindi and regional languages across all camps and village meetings for spreading the awareness.
A letter from Hon’ble Prime Minister was sent to all beneficiary families to make them aware about their entitlements under the scheme and also provide them a family card with unique family ID. Standardised design materials have been prepared by NHA that are being used by States for making beneficiaries aware about the scheme. Various communication channels like print media, television, radio, social media etc. are being used to reach beneficiaries and other stakeholders. A communication strategy and IEC guidebook has also been developed for this purpose. A dedicated web portal for the scheme www.pmjay.gov.in has been also created to provide all the details about the scheme to various stakeholders. All relevant information and links e.g. list of empanelled hospitals, Am I eligible portal, grievance redressal portal, gallery, operational guidelines are placed here.
Support Systems
Apart from above mentioned critical components of PM-JAY’s ecosystem following are some other key components working as the support system for the smooth implementation of the scheme.
Capacity DevelopmentCapacity building activities under PM-JAY attempt to address more than just training and cover all aspects of building and developing sustainable and robust institutions and human resource. Capacity building in PM-JAY has three components:
- Setting up sustainable institutional structures,
- Building and strengthening the human resource and institutional capacity, and
- Sustaining knowledge and skill through knowledge management and use of appropriate tools. The roles of institution as well as each of its personnel at national, State and district level were defined as were their specific skill sets required. These personnel were further categorised on the basis of role and appropriate knowledge and skill areas were mapped for capacity development.
The NHA has taken the leadership role in assessing the requirements, making available resources, devising strategies for enabling States to undertake capacity building activities and providing technical assistance to States. Standardised learning content on identified thematic areas is being developed by the NHA. States can customise these materials and deliver through various methodologies as per their annual training plan. Monitoring and quality assurance measures with feedback mechanism have also been put in place to ensure effectiveness and efficiency. Partnerships and networks are being created with Government and non-Government institutions having expertise in various fields to support the capacity building initiatives in PM-JAY.
Capacity building initiatives in PM-JAY started with the orientation of SHA officials followed by various workshops for personnel from specific portfolios like IT, fraud control, claim management, etc. Workshops for ISAs and banking partners were also organised. Master trainers were created at the State level who in turn trained more than 10,000 Pradhan Mantri Arogya Mitras (PMAMs) at empanelled hospitals before the beginning of the programme. Learning materials were also made available in the portal to facilitate State and district level trainings. An e-learning platform is now being developed with the support of the National Skill Development Council (NSDC) for training and certifying Arogya Mitras. Various workshops, cross learning forums and thematic trainings are planned in the upcoming days.
Monitoring and EvaluationMonitoring and Evaluation under PM-JAY Monitoring and Evaluation (M&E) is key for successful implementation and ensuring the intended results of such a large insurance scheme. The NHA at the Central level is continuously keeping track on periodic basis on these UHC dimensions (coverage, benefits and financial protection) through the following functional domains:
- Beneficiary management
- Transaction management
- Provider management
- Support function management (comprising functions such as capacity development, grievances, frauds and abuse, call centre, etc.)
A strong real-time online MIS is set up at the national level to review Key Performance Indicators (KPIs) and achievement of results with respect to the targets defined under the domains. The various dashboards developed using business intelligence tools help in identifying the gaps and provide an overview of the performance made. To mention a few: the operations dashboard presents an update of KPIs of beneficiary information system, pre-auth dashboard helps to access state and district wise distribution of pre-auth, status of empanelled hospitals, portability dashboard gives us the picture of interstate and intrastate portability and their KPIs on claim portability by specialty, procedure, age and gender.
Most of the States, which do not have their own schemes, are using the NHA software. However, States with their own schemes are either using the above or their own software followed by API integration to ensure the flow of data from State to Central servers.
In order to provide a comprehensive picture of the progress made by all the functional domains, factsheets are developed monthly at the State and National level. The factsheet compares the progress made since the inception of the scheme across States with the progress made in each month. The average claim size, total number of pre-auths generated, pending approvals, nomenclature of the packages used at public and private facilities are some of the important indicators included in the factsheet. The triggers and outliers (if any) identified through the dashboards and factsheet are further drill down to districts level.
To assess and comprehend the impact of PM-JAY, evidence generation is done through evaluation studies in collaboration with premiere research institutions and in partnership with development agencies such as GIZ, WHO and World Bank. The objective of these evaluation studies is to understand the impact of the scheme on various parameters including but not limited to out-of-pocket expenditure, access to health, health seeking behaviour, etc. These research studies provide critical inputs for evidence-based decision-making and carrying out mid-course corrections.
Fraud Prevention, Detection and ControlFor a programme of this scale, magnitude and complexity as that of PM-JAY, it is critical to put in a place a strong anti-fraud mechanism not only from financial perspective but also to safeguard people’s health from unethical behaviour and malpractices. The National Health Authority is cognizant of the issue and has taken a number of steps to safeguard the programme from the inception. Some of the key actions taken in this regard are listed below.
- A transparent tendering process implemented for selection of insurance company, Implementing Support Agency and other service providers. Tightly worded legal document for service delivery as per pre-defined Service Level Agreements have been developed with penalty clauses and punitive action to deal with fraudulent activities on the part of any agency involved in delivering services under PM-JAY.
- Hospital empanelment process has been developed with a two-tiered structure approach involving district level and State level committees, having due representation of senior officials – civil surgeon, chief medical officer and nodal officers of the district. The entire process is web enabled whereby a hospital can track the status of its empanelment from application to approval by the State Nodal Age.
- IT system and processes have been designed with checks and balances along with defined roles and responsibilities, role-based logins and audit trails for all processes – beneficiary identification, transaction management system, funds flow, claims payment etc. Further, all pre-authorisation and claims transactions are carried out on-line basis for efficiency and complete transparency.
- The process of pre-authorisation has been designed such as to ensure maximum efficiency while avoiding abuse and fraud. Minimum requirements for claims investigation and medical audit have been laid down.
- The tendency of health care providers to overcharge, bill extra and other related issues have been taken care of by introducing all-inclusive package rates. However sufficient flexibility has been given to treat patients requiring medical management and the list for procedures shall be enhanced as more experience and insights are gained.
- Comprehensive Anti-fraud Guidelines were released by the Minister of Health and Family Welfare on August 27, 2018, laying down detailed strategy, processes, systems and manpower for anti-fraud both at National and State levels.
- National Health Agency Tollfree – 14555 set up on 24×7 basis for facilitating beneficiary reporting and feedback
- Whistleblower Policy has been adopted at the NHA level and shared with States for adoption on a similar pattern
B. Operational and System Level
- Capacity building workshop for fraud control and medical audit organised for SHAs, ISAs and Insurance partners
- Fraud Investigation Manual released for uniform and effective process, data capture
- Monitoring and analysis of utilisation trends done through regular MIS and dashboards, watching abuse prone packages, suspect transactions/hospitals on regular basis
- Top analytics firms shortlisted for carrying out ‘proof of concept’ for triggering suspect transactions and entities through rule engines and artificial intelligence layer on top of Transaction Management System
- Mobile App – Kaizala app is being customised for field investigations and medical audit, test deployment underway
- Procedure specific documentation and checklist being developed for controlling abuse and leakages, integration with IT underway
- Adjudication guidelines and capacity building programme for SHAs, ISAs to be rolled out
- Watch and action against fake websites, Mobile Apps providing misleading information or collecting money or data from public
NHA has a “Zero Tolerance” approach towards Fraud and Abuse under PMJAY. Towards this end, the National Anti Fraud Unit (NAFU) has been set up with the primary responsibility for prevention, detection and deterrence of fraud and abuse under PM-JAY.
NAFU works closely with State Ant Fraud Units (SAFU) in order to ensure the effective implementation of the Scheme, free from any fraudulent/ abusive activity from any entity involved in PM-JAY implementation such as providers, beneficiaries, ISAs or payers.
NAFU carries our following key activities:
- Provide leadership stewardship to the national anti-fraud efforts under PMJAY;
- Develop, review and update the national anti-fraud framework and guidelines based on emerging trends;
- Provide mentoring support to states in setting up and institutionalising their in-state anti- fraud efforts;
- Capacity building of states on anti-fraud measures under PMJAY;
- Liaise with the national IT team / agency to ensure that the IT platform is periodically updated with fraud triggers based on review of trends;
- Conduct audits and investigation of suspect cases/entities;
- Set up Forensics practice for detection and triangulating fraud/abuse related data with the overall service utilisation trends emerging under PMJAY;
- Provide evidence-based insights to states on trends emerging from state-specific fraud data analytics;
- Handle all fraud related complaints that the NHA may receive directly and liaise with the states from any complaints specific to states as per Anti- Fraud Guidelines
- Establish whistle blower mechanism, public disclosure guidelines, and other deterrent measures.
Grievance redressal system is designed to address grievances of all PM-JAY stakeholders based on the principles of natural justice while ensuring cashless access to timely and quality care remains uncompromised. A three-tier Grievance Redressal Committee structure has been set up at National, State and district levels for this purpose. The CEO of NHA will be the Chairperson at the National level while the CEO of SHA will chair the State Grievance Redressal Committee. The District Magistrate or an officer of the rank of Additional District Magistrate shall be the Chairperson of the District Grievance Redressal Committee. These committees will track and monitor the grievances and its status, collect additional information from parties involved, facilitate hearings, review records, adjudicate and issue orders on grievance and ensure compliance of committee orders.
The aggrieved parties can submit grievances through offline (letter) or through an online portal (https://cgrms.pmjay.gov.in) developed by NHA. Other communication channels like telephone call, fax, e-mails, and SMS are also accepted for registering a grievance. The National Call Centre (14555 / 1800 111 565) is also integrated to the Grievance Portal for addressing grievances received through the call-centre. The committee can also register grievances based on social media or public forums findings/reports. Based on predefined criteria, grievances will be handled either by the respective individual/organisation who is responsible to take action or by the committees at an appropriate level. But at any level, the grievance should be addressed within 30 days of receipt. The right to appeal for any party is valid for 30 days from the date of the decision. Non-compliance with the decisions of the committee within another 30 days will also attract a penalty for the defaulter. The online portal has the provisions to designate and track grievances to respective officials and monitor compliance with the alert system.
Call CentreOne of the important aspects of one of the world’s largest government-supported health schemes of the size and complexity as that of PM-JAY is to ensure that entitled beneficiaries of the programme can reach out to know the details of the scheme, have recourse to raise a query or a grievance, seek information and support at any time during day or night, especially during hour of need. If the profile of beneficiaries includes a sizeable population which is rural based, even less educated and less aware, the mechanism needs to be further simplified and made easily accessible, involving least effort and no expense. Therefore, a National Helpline – 14555 was set up by then National Health Agency on August 24, 2018 – which is operating 24×7 since the launch and has answered more than 42 lakh calls since inception. The call centre is manned by 300 plus trained agents who work round the clock to manage the calls and further plans are in offing to expand capacity. All major regional languages are supported by the call centre team.
The Helpline is toll-free which means that the caller does not incur any call charges, the same are borne by NHA. Operating on 24x7x365 basis, the call centre provides services/information to the beneficiaries such as details about the scheme – coverage, benefits, how and where to avail benefits, name and address of empanelled hospitals etc. Besides beneficiaries, other stakeholders like hospitals, Arogya Mitras and field functionaries also call the Helpline for support.
The call centre is also engaged in outbound calling and more than 3 lakh outbound calls have been made to beneficiaries for collecting their feedback post discharge from hospital, to know their experience, whether any difficulty faced during the process, etc. Outbound calls are also made to hospitals to help them complete application for support, hand-holding and training for providing services to PM-JAY beneficiaries and to encourage these hospitals to raise pre-authorisation.
Convergence
The National Health Authority (NHA) has entered into a partnership with the Employee’s State Insurance Corporation (ESIC). This synergy between Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (AB PM-JAY)and Employees State Insurance Scheme (ESIS) will create an ecosystem wherein ESIC beneficiaries will be able to access services at ABPM-JAY empanelled hospitals and vice versa.
The convergence between PM-JAY and ESIC is a landmark initiative for the development of health systems in the country. This will leverage the presence of an established network of quality services providers under PM-JAY alongside fixed health benefit packages, thereby standardising services across schemes. Further, it will create higher demand for health services at ESIC empanelled hospitals that may be currently underutilised. This will support in improvement of infrastructure and facilities of such facilities, via utilisation of funds reimbursed under PMJAY.
In the initial phase, a pilot is being conducted in Ahmednagar, Maharashtra and Bidar, Karnataka wherein ESIC beneficiaries of these districts will be able to access PM-JAY services in PM-JAY empanelled hospitals. The beneficiaries will be eligible for all 1,929 secondary and tertiary packages under the scheme and the initiative will be scaled up to 102 districts with a plan of eventually extending coverage across the country.
Key Benefits of AB PM-JAY and ESIS convergence:- ESIC beneficiaries will get access to healthcare providers under AB PM-JAY
- AB PM-JAY beneficiaries will be able to avail services in ESIC empanelled hospitals.
- Beneficiaries of ESIC can use their ESIS card to access free treatment at AB PM-JAY empanelled hospitals.
- Similarly, beneficiaries of AB PM-JAY can use their PM-JAY card to access free treatment at ESIC empanelled hospitals.
What is a Medical Termination of Pregnancy (MTP)? Medical termination of pregnancy (MTP), commonly known as abortion, is a procedure to end a pregnancy. It can be performed either through medication (medical abortion) or a surgical procedure (surgical abortion), depending on the pregnancy duration and the woman’s overall health. In India, abortion is legally permitted under specific conditions, and licensed MTP centers are authorized to provide these services safely and in a regulated environment.
Worried About Pregnancy?
Missed Abortion?
Get Medical Termination of Pregnancy (MTP)
100% Legal: All legalities and paperwork completed as per the MTP Act before any procedure. 100% Confidential Safe Procedure
Medical Termination of Pregnancy (MTP)
MTP is a legal procedure to terminate a pregnancy using medications. In the early stages of pregnancy (0-7 weeks), it can be terminated with medicine. Beyond this period, a surgical process may be needed.
0 – 7 Weeks Pregnancy
Abortion, the ending of a pregnancy by removal or expulsion of an embryo or fetus before it can survive outside the uterus, can be done through a medical abortion (medication abortion) using pills. Medically treated No hospitalization required 100% safe, legal, and trustworthy Affordable rates for all sections of society
*Treatment procedures may vary from patient to patient.
7 – 12 Weeks Pregnancy
Dilation and Curettage (D&C) involves the dilation (opening) of the cervix and the surgical removal of part of the lining of the uterus and/or contents of the uterus by scraping and scooping (curettage). It is a common method for first trimester miscarriage or abortion.
- Day care procedure (no overnight stay required)
- No scarring
- No hospitalization required
- 100% safe, legal, and trustworthy
*Treatment procedures may vary from patient to patient. The final decision will be made by the doctor after a thorough examination.
Who Should Not Choose MTP?
Women should avoid medical abortion if they have any of the following conditions: Heart or blood vessel complications Uncontrolled seizure disorder Ovarian mass or anemia Allergy to the medications involved If the pregnancy period exceeds 9 weeks, a medical abortion should be avoided.

